
Obtaining a reliable pulse-oximetry reading may be challenging if a patient’s fingers are constricted or they do not remain still. Patients with panic-induced hyperventilation should be well oxygenated and have a pulse-oximetry reading above 95%. Pulse-oximetry and waveform capnography are valuable tools to assess patients with hyperventilation syndrome, but they also have limitations. Vasospasm associated with respiratory alkalosis can also trigger acute coronary syndromes. Remember that other conditions may have been misdiagnosed as panic attacks in the past, and also that pulmonary embolism, sepsis, diabetic ketoacidosis can cause hyperventilation in young and otherwise healthy people. Patients also often have a history of panic attacks and can compare their present symptoms to previous ones. Panic attacks usually have a precipitating event, such as an argument, bad news or a phobia, but they do not always have an identifiable trigger.
#Normal range of capnography how to
Understand how to interpret assessment findings in hyperventilating patientsĪlways start your assessment by look for life-threatening causes of hyperventilation, and panic-induced hyperventilation should always be a diagnosis of exclusion. Hyperventilation associated with these conditions is caused by the body compensating for an underlying problem, which will be made worse if the patient reduces their respiratory rate. Elevated respiratory rate, difficulty breathing, anxiety, chest discomfort, diaphoresis, syncope, and extremity spasms can be caused by other life-threatening conditions, including: Panic attacks are only one cause of hyperventilation. Hyperventilation is also a response to respiratory, perfusion or metabolic compromise When triggered by a panic attack, the patient’s symptoms improve and the electrolyte levels normalize once they slow their respiratory rate. Calcium levels also decrease in respiratory alkalosis, which can cause numbness, tingling and spasms of the patient’s hands and feet, known as carpopedal spasm. Acute respiratory alkalosis also causes cerebral vasoconstriction and decreased blood supply to the brain, which can lead to syncope and altered mental status.
Hypocapnea leads to respiratory alkalosis, which causes oxygen to bind more strongly to hemoglobin and less is released for tissue perfusion.

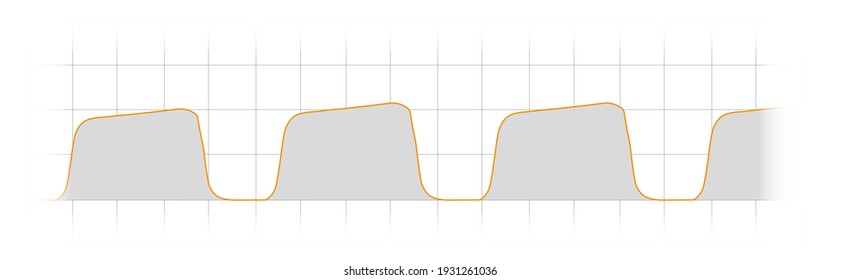
Panic-induced hyperventilation causes more carbon dioxide to be exhaled than the body can produce, which decreases the partial pressure of CO2 in the bloodstream (PaCO2), or hypocapnea. The patient then feels like they need to breathe even faster and deeper, leading to a cycle of worsening anxiety and respiratory distress. This leaves little room for the chest to expand and the patient feels like they are suffocating. Panic attacks progress to hyperventilation syndrome when patients continue to breathe faster than they are able to control, and use chest muscles rather than their diaphragm for ventilation. It is closely related to panic attacks, where the patient experiences a sudden onset of intense fear, with or without an identified trigger, along with physical symptoms including: Hyperventilation syndrome is a condition in which a patient’s respiratory rate exceeds the body’s metabolic demands for oxygen and carbon dioxide. Hyperventilation syndrome is primarily a respiratory problem triggered by panic Here are four things to know to identify and treat panic-induced hyperventilation syndrome.

Hyperventilation is also a sign of several life-threatening metabolic, respiratory and circulatory conditions, which can present with similar assessment findings and vital signs as panic-induced hyperventilation. When triggered by anxiety, hyperventilation causes patients to feel like they are suffocating, but it eventually self-corrects and is physiologically benign. Hyperventilation syndrome is a challenging and often misunderstood condition that is frequently encountered in EMS.


 0 kommentar(er)
0 kommentar(er)
